Basic Cardio Tests
Electrocardiogram (ECG) records the electrical activity of the heart, shows abnormal rhythms (arrhythmias), and can sometimes detect heart muscle damage. The ECG machine detects tiny electrical signals that make your heart pump blood around your body. The ECG machine does not put any electricity into your body.
An ECG test takes about 5-10 minutes. Small metal electrodes are placed on your arms, legs, and chest. Wires connect these electrodes to the ECG machine. This machine detects the electrical signals that start each heartbeat and records them onto paper or a computer. During the test, you lie quietly on a table while the machine records your heart’s electrical activity. You will need to lie as still as possible, without talking, and breathe normally. After the procedure, the electrodes are removed and discarded. The ECG is painless and harmless.
An ECG is done to: help find the cause of palpitations or chest pain, dizziness, shortness of breath or fainting, check how well medicines are working and their effect on the heart, check how well mechanical devices that are implanted in the heart, such as pacemakers, are working to control abnormal heart activity.
Sometimes an ECG is done as part of routine tests, like before an operation.

A Transthoracic Echocardiogram (echo or TTE) is a noninvasive test that uses sound waves to evaluate your heart’s chambers and valves, and how well it pumps. The echo sound waves create a real time image on the monitor as an ultrasound probe is passed across the skin over your heart.
An echo uses soundwaves to look at the structure, function and size of your heart. You might need this test to see if you have heart related disease or heart failure. A transthoracic echocardiogram is a standard echocardiogram where the heart is scanned using a small wand that is moved across the surface of your chest. How do I get ready? No special preparation is required. You will need to undress to the waist in a private space and a hospital gown will be provided.
The technician places a wand on different areas of your chest. The wand sends out sound waves that produce an echo image of the heart walls and valves on the computer screen. The test will take about 15-20 minutes.
There are no significant risks involved in a standard transthoracic echocardiogram. You may feel some discomfort like pulling off an adhesive bandage when the technician removes the electrodes placed on your chest during the procedure.

This is also called a treadmill or exercise ECG. This test is done to monitor the heart while you walk on a treadmill or pedal a stationary bike. Your doctor also monitors your breathing and blood pressure. A stress test may be used to detect coronary artery disease, or to determine safe levels of exercise after a heart attack or heart surgery.
It is an ergometric stress test that is used to identify or exclude ischemic heart disease. The patient is submitted to physical exercise, usually on a treadmill or stationary bicycle, in order to increase his heart rate. As the pulse rate rises, the ECG records changes that may occur. These changes could be evidence of cardiac distress related to an oxygen deficit.
If the stress test is indicative of ischemia, physicians can build a plan of care that might include anything from diet management to medications and even surgical interventions. At specific intervals after the interventions are put in place, the patient will submit to subsequent ergometric stress tests to measure how well the interventions are working.

For this test (24 or 48-hour cardiac Holter monitoring), you wear a small, portable, battery-powered ECG machine. Small patches (wired electrodes) are attached to the skin over your heart.
The monitor to records heartbeats over a period of 24 to 48 hours during normal activities. At the end of the time, you will return the monitor to the doctor’s office so it can be read and evaluated.
It is important to record your daily activities (mealtimes, exercise, bedtime) and any symptoms you feel. Please remember: Don’t touch or adjust the electrodes. Don’t get the electrodes or monitor wet (don’t swim, shower or bathe). Don’t have an X-ray. Avoid using an electric blanket.
There are no significant risks involved in wearing a Holter monitor. However, you may have some skin irritation around the electrodes.

Blood pressure (BP) monitoring involves regular blood pressure recordings over a day.
A BP cuff is worn on your upper arm and connected to a monitor. The monitor is worn on a strap over your shoulder. Your heart rate and BP are measured every hour during the day and every two hours at night. During each measurement, the BP cuff will get tight and then slowly loosen again.
When the cuff is at its tightest, it closes off an artery before slowly re-opening it. This allows the blood pressure unit to measure how quickly blood refills this artery. It will take about 15 minutes to have the cuff put on and to get instructions.
You will need to return to the hospital the next day at the same time (24 hours later) to have the monitor taken off. There are no significant risks involved in 24-hour BP monitoring.

At Polyclinic Glorieta in Dénia we have incorporated a Sleep Unit, very important for the diagnosis of apnea. This novelty will strengthen patient care and also have treatment without hospital admission.
Obstructive sleep apnoea (OSA) is a common disorder characterized by repetitive episodes of nocturnal breathing cessation due to upper airway collapse. OSA causes severe symptoms, such as excessive daytime somnolence, and is associated with a significant cardiovascular morbidity and mortality. Different treatment options are now available for an effective management of this disease. After more than three decades from its first use, continuous positive airway pressure (CPAP) is recognized as the gold standard treatment. Nasal CPAP (nCPAP) is highly effective in controlling symptoms, improving quality of life and reducing the clinical sequelae of sleep apnoea. Other positive airway pressure modalities are available for patients intolerant to CPAP or requiring high levels of positive pressure. Mandibular advancement devices, particularly if custom made, are effective in mild to moderate OSA and provide a viable alternative for patients intolerant to CPAP therapy.
Thus, in Glorieta Polyclinic we have a modern home respiratory polygraphy, without the need for hospital admission, which can take the patient home and sleep comfortably with it, requiring a record of not less than 6.5 hours and must include at least 3 hours of sleep, and we work with the best apnea specialists, RESMED.

Special Eco tests
Also called an echocardiography stress test or stress echo, is a procedure that determines how well your heart and blood vessels are working. During a stress echocardiography, you’ll exercise on a treadmill or stationary bike while your doctor monitors your blood pressure and heart rhythm.
When your heart rate reaches peak levels, your doctor will take ultrasound images of your heart to determine whether your heart muscles are getting enough blood and oxygen while you exercise.
Your doctor may order a stress echocardiography test if you have chest pain that they think is due to coronary artery disease or a myocardial infarction, which is a heart attack. This test also determines how much exercise you can safely tolerate if you are in cardiac rehabilitation.
The test can also tell your doctor how well treatments such as bypass grafting, angioplasty, and anti-anginal or antiarrhythmic medications are working.

This test is for people who cannot exercise on a treadmill or an exercise bike. It involves giving you a drug called dobutamine, which makes your heart beat faster to mimic the effects of exercise on the heart. The specialist can then use an echocardiogram (echo) to assess how well your heart is working and recommend suitable treatment options.
Small electrodes are placed on your chest to monitor the rate and rhythm of your heart. Your blood pressure is also monitored. The technician places a wand on different areas of your chest. The wand sends out sound waves that produce echo images on the computer screen. An intravenous (IV) line is inserted into your arm so the dobutamine can go straight into your bloodstream. The IV line is taken out when all the drug is in your bloodstream. The test takes about one hour but you may be in the policlinic for about 90 minutes.
There are eating and drinking restrictions for this test: Avoid drinking caffeine (coffee, tea, cola) but you may drink water, do not eat for a minimum of four hours before the test, and wear comfortable clothing.

This test is like a transthoracic echocardiogram. But it is done with medicine to help you relax (sedation). It is more invasive because a probe is put into your body. In this test, you will swallow a small probe about the size of your thumb. The probe passes down the esophagus, which lies directly behind the heart. It allows a much closer look at the heart’s structure and function than a standard echocardiogram done on the skin of the chest. It can better look at heart valve structure and function. Your healthcare provider can better see any blood clots that may be in the heart.
In a transoesophageal echocardiogram (TOE), a scanner is used to view the heart from within the gullet (oesophagus), just behind the heart. This can give a better view of the heart than a standard echocardiogram.
You will be given a calming drug through an IV line inserted in your arm. Saline or a dye may be used to help get a clearer echo image. A device to measure the oxygen in your blood may be attached to your finger or earlobe. Your heart rate, breathing rate and blood pressure are monitored throughout. An anaesthetic spray is used to numb your throat. The spray may taste bitter and make your tongue and throat feel numb and swollen. Remember to relax and take deep breaths. You will lie on your left side with your head tilted forward. A mouthguard will protect your teeth. A thin tube with a probe will be guided down your throat into your gullet.
After the test, your nurse will tell you when you can eat and drink again. Once you are discharged from the hospital, you will not be able to drive for the rest of the day because of the anaesthetic. You should get someone to drive you home.

Arrhythmias
Electrical cardioversion also called direct current (DC) cardioversion, is a short procedure which uses a defibrillator to provide an electrical shock to the heart. It is performed in a hospital under sedation or anaesthetic.
The defibrillator sends an electrical impulse through your chest wall, via pads or electrodes which are placed on your chest. This impulse disrupts the abnormal rhythm for a split second, allowing your heart to resume a normal rhythm. The procedure takes a few minutes and because of the sedation you shouldn’t feel any discomfort. Most people are able to go home from hospital the same day.
Pharmacological cardioversion, also known as chemical cardioversion, uses medicines called anti-arrhythmic to restore a normal heart rhythm. Your healthcare professional may give you these anti-arrhythmics in an oral form (tablet) or intravenously (through a vein). This procedure will also be carried out in hospital and your heart rhythm will be monitored closely throughout.
It is also important to remember that cardioversion doesn’t always work. For some people, their heart won’t return to a normal rhythm. Others may slip back into atrial fibrillation later.
Even if your heart does return to a normal rhythm, you will still need to take medication to prevent blood clots because you are still at a higher risk of having a stroke.

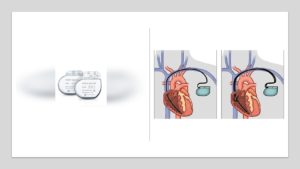
Pacemakers can be used to treat slow or irregular heartbeats called arrhythmias.
Your heart beats regularly and at different rates depending on your body’s needs. This is controlled by your heart’s electrical conduction system.
A pacemaker is sometimes used to correct slow or irregular heartbeats called arrhythmias. These arrhythmias may cause you to feel light-headed, breathless, or even experience blackouts. If your heart rate is too slow, the pacemaker will send an electrical signal to the heart muscle to start a heartbeat. You are unlikely to feel your pacemaker when it activates so don’t let this worry you. When your heart is beating normally, the pacemaker will not be activated.
Pacemakers are made up of a long-lasting battery and an electronic circuit in a metal case that sits under your skin. The pacemaker is connected to your heart muscle by one or two leads. Modern pacemakers can be very reliable and comfortable.
Having a pacemaker can greatly improve your quality of life and for some people it can be lifesaving. A pacemaker can relieve some arrhythmia symptoms, such as fatigue and fainting. A pacemaker may help a person with abnormal heart rhythms to resume a more active lifestyle.
There are several types of pacemaker available. Together with your doctor, ask about the options and talk about what may work best for you.
This device is about the size of a AAA battery. Your doctor puts the device under the skin over the heart. The device monitors and records heartbeats for up to 3 years.
The implantable loop recorder is a tiny monitor, about the size of a piece of chewing gum, which can be implanted under the skin and used to record heart rhythm abnormalities. It is inserted during a 15-20-minute minor surgical procedure performed under local anaesthetic.
It can be used for people whose atrial fibrillation episodes can’t be captured by a holter monitor or external event recorder, because the gaps between the events are too long.
This device is an implantable patient-activated and automatically-activated monitoring system that records subcutaneous ECG and is indicated in the following cases: a) patients with clinical syndromes or situations at increased risk of cardiac arrhythmias; b) patients who experience transient symptoms such as dizziness, palpitation, syncope and chest pain, that may suggest a cardiac arrhythmia.
This Holter is placed under the skin in the upper chest area. Slim-shaped, leadless device simplifies insertion. The recommended implant zones are from the left parasternal area extending to the mid-clavicular line between the first intercostal space and the fourth rib (choose a site as near to the sternum as possible). The lower chest V3 area, between the fourth and fifth rib, is an alternative implant site. The exact location may vary from this diagram due to the patient’s anatomy.
During the brief procedure, the area is numbed with local anaesthesia, a small incision is made, and the monitor is inserted.
Easy access to diagnostic data without an in-office clinic visit – optimizes scheduling and treatment. Data may be transmitted immediately after patient-marked event or at scheduled intervals.
We are currently working with two major world companies specialised in the field of arrhythmias, namely MEDTRONIC (USA) and BIOTRONIK (Germany), and we have been honoured that the Glorieta Dénia Polyclinic is the first centre in Spain to implant the new model of remote insertable subcutaneous Holter by Biotronik, in particular the IIIm, which is characterized by the longest battery life (over 5 years), small size, easy insertion, and transmission of very good ECG records that facilitate reading and compression of the ECGs.

Rehabilitation and sport
Cardiac rehabilitation is a programme that supports your recovery and ongoing wellbeing after a heart event or heart disease diagnosis. It reduces your risk of future heart events and improves your quality of life. Cardiac rehabilitation (cardiac rehab) is a programme of education, training and support for people who have had a heart event.
Cardiac rehabilitation will: (1) Reduce the likelihood of readmission following your surgery or heart event. (2) Lower your risk of future heart events. Improve your quality of life
The main aim is to get you back to as full a life as possible by promoting your health and keeping you well after you leave hospital.
Cardiac rehab can be beneficial if you: Have had a heart attack. Have had coronary angioplasty (stent). Have had coronary bypass surgery or another type of heart surgery. Have stable heart failure.
Ideally you should start your cardiac rehabilitation within a few weeks of your discharge from hospital. But even if you’re some time past that, cardiac rehabilitation will still be of benefit. It’s never too late to start.
Our REMA Clinic in Denia is the first clinic specialized in Cardiac Rehabilitation in our area, with specialists in the field, with all the technology and preparation to fully assist you.

Sports cardiology is an advancing field that encompasses the care of athletes and active individuals with known or previously undiagnosed cardiovascular conditions. It incorporates many aspects of cardiology, such as cardiac imaging, electrophysiology, structural heart disease and exercise physiology.
In Denia we have a complete personal and technological team to carry out the best sports cardiology. Many sports clubs have agreements with us, so we work with amateur, semi-professional and professional athletes, even with people who want to start doing sports, because sport is health, but always with medical control.
As such, a comprehensive sports cardiology program should include physicians with specific knowledge within these fields. The sports cardiology team should include those with expertise in the paediatric heart, especially congenital heart disease and inherited diseases, cardiovascular imagers, electrophysiologists, heart failure specialists and exercise physiologists. These specialists must come together to make comprehensive assessments and recommendations for athletes.
Examples include the assessment of exercise-induced cardiac remodelling versus cardiac pathology, the utilization of cardiac MRI, CT and cardiopulmonary exercise testing (CPET) specific for athletic patients, accessing genetic counselling when appropriate, and the determination of sports eligibility and exercise prescriptions for athletes with cardiovascular risk and disease.
A close relationship with athletic trainers, coaches, and families is also necessary to maintain a multidisciplinary approach to the care of the athlete. The sports cardiology team will help athletes make informed decisions to allow them to participate in sport safely and effectively.

